The Cancer Conversations series with Mayo Clinic medical experts, community members, patients, and survivors, offers valuable education on prevalent cancers, including prevention, screening, research, and treatment options.
The recent community discussion about liver cancer, featured Dr. Lionel Kankeu Fonkoua, an oncologist with the Mayo Clinic Comprehensive Cancer Center who specializes in the treatment of gastrointestinal and liver cancers. He is also a Robert Winn Career Development Award recipient dedicated to helping minority and at-risk patients through research and clinical trials.
"It's a program that's designed to make sure that those clinical trials are community designed, conducted and informed to make sure that whatever research we do, we have the intent from the get-go of thinking about the communities that are at risk, vulnerable and most likely to benefit," says Dr. Kankeu Fonkoua.
The Big Takeaway: Early Detection Saves Lives
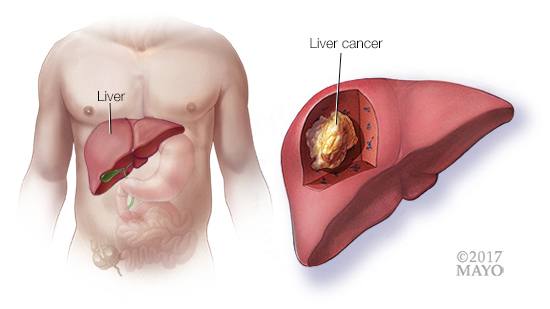
Liver cancer is the sixth most common cancer worldwide and a leading cause of cancer-related deaths, with survival rates still very low. Unfortunately, most patients are diagnosed too late for curative treatments, making early screening vital. Certain racial and ethnic groups—such as Black, Hispanic, Asian, and Native American populations—face a much higher risk due to disparities in healthcare access and higher prevalence of risk factors.
How Does Liver Cancer Develop?
Liver cancer usually results from chronic liver inflammation, which leads to cirrhosis (scarring of the liver). Major risk factors include:
-
Hepatitis B & C infections
-
Alcohol-related liver disease
-
Fatty liver disease (linked to obesity and diabetes)
Hepatitis B is especially concerning because it can lead directly to liver cancer without first causing cirrhosis. This makes regular screenings crucial for those at risk.
How Do Doctors Detect Liver Disease and Cancer?
Doctors start with blood tests, checking:
- Liver function – Elevated bilirubin (linked to jaundice) and low albumin suggest poor liver health.
- Platelet count – A low count signals worsening cirrhosis and increases bleeding risk.
- Alpha-fetoprotein (AFP) – A tumor marker; high levels in 75% of liver cancer cases suggest malignancy.
If liver cancer is suspected, imaging tests come next:
- Ultrasound – A quick, affordable first step to detect abnormalities.
- CT scan or MRI – More detailed imaging to confirm liver damage or tumors.
- Biopsy – Sometimes needed for genetic testing, but in most cases, liver cancer can be diagnosed with imaging alone.
How Liver Cancer Progresses
Liver cancer can start as a small lesion and grow into more serious stages:
-
Early Stage – A small tumor (less than 2 cm).
-
Intermediate Stage – Multiple tumors in different areas of the liver.
-
Advanced Stage – The tumor spreads to blood vessels or nearby organs.
-
Late Stage – The cancer has spread beyond the liver.
How is Liver Cancer is Treated?
Treatment depends on how early the cancer is caught and the overall health of the liver.
-
Curative Treatments (For Early-Stage Liver Cancer)
-
Surgery (Liver Resection): Removes the cancerous part of the liver. Only an option for patients with good liver function.
-
Liver Transplant: Completely replaces the diseased liver with a healthy one. This is the best cure but requires a donor organ and a long waiting list.
-
-
Targeted Treatments (For Intermediate or Advanced Stages)
-
Ablation Therapy: Uses heat or cold to destroy cancer cells in small tumors.
-
Transarterial Chemoembolization (TACE): Injects chemotherapy directly into the tumor while cutting off its blood supply.
-
Transarterial Radioembolization (TARE): Similar to TACE but uses radiation instead of chemotherapy.
-
-
Systemic Treatments (For Advanced and Metastatic Stages)
-
Immunotherapy: Boosts the body’s immune system to fight cancer.
-
Targeted Therapy: Uses drugs that block cancer growth at a molecular level.
-
Chemotherapy: Less effective for liver cancer but sometimes used in later stages.
-
-
Palliative Care (For End-Stage Disease)
-
When liver cancer is too advanced for treatment, care focuses on pain relief and quality of life.
-
Liver cancer disproportionately affects racial and ethnic minority communities, especially those who are underinsured or lack access to consistent healthcare. Studies show that African individuals—particularly those born in Africa (except North Africa)—face an even higher risk of developing liver cancer at an early age, often before 40. This means that not only do these communities experience higher rates of the disease, but they also get diagnosed later when treatment options are limited.
This disparity is due to multiple factors:
-
Lack of routine screenings due to healthcare access barriers.
-
Higher rates of underlying conditions like hepatitis B and C, which increase liver cancer risk.
-
Limited awareness of the importance of early detection.
Many patients in underserved Black and African communities, are not screened early enough. By the time they seek medical attention, the disease is often in an advanced or late stage, when treatment options are limited. If liver cancer is caught early, it can often be cured with surgery or other treatments. That’s why outreach and education are so important—especially in at-risk minority communities.

Dr. Kankeu Fonkoua is leading a clinical trial through the Robert A. Winn Diversity in Clinical Trials Award Program, which focuses on the immigrant African and Asian communities of Minnesota with a high prevalence of hepatitis-induced hepatocellular carcinoma — a type of liver cancer.
"This is an at-risk population that we are intentionally targeting, because they are not represented in a lot of our immunotherapy trials," he explains.
"It's very important to make sure that the at-risk population — the vulnerable population that's going to most likely benefit the most from the therapy — is represented. Because you have to tell them (and) it's hard to tell a patient this is a study, a clinical trial, that had 1,000 patients, (and) only 1% to 2% were actually like you," says Dr. Kankeu Fonkoua.
 Connect
Connect
 Connect
Connect
My cancer started in the colon, progressed to the liver and I have just been informed that there are now 4 spots on my lungs, 2 of which are considered to be cancerous. The advice I have received via Mayo during this journey has been magnificent and I would now welcome further advice concerning my lungs.
I recovered very well from the colon and liver resections and I'm currently 100% fit - lots of skiing, cycling and walking so far this year. But I've been informed I will most likely need chemotherapy and ablation treatment for the lungs.
Could someone tell me about their experiences of ablation treatment and whether this was done before or after chemotherapy? And is the cancer likely to spread elsewhere too? Many thanks.
@martin77, that is a good topic for a new discussion in the Liver Cancer support group: https://connect.mayoclinic.org/group/liver-cancer/
In the meantime, you may wish to read this related discussion in the Pancreatic Cancer group where members are talking about liver ablation:
- Radio frequency ablation in liver Mets
https://connect.mayoclinic.org/discussion/radio-frequency-ablation-in-liver-mets/